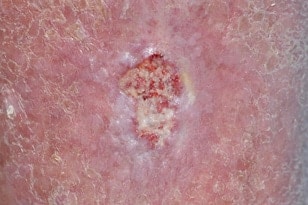
Squamous Cell Carcinoma Basics
Squamous Cell Carcinoma is the second most common type of skin cancer. It is caused by DNA damage that leads to abnormal changes in the squamous cells in the outermost layer of skin.
It most commonly appears on the face, scalp, ears and backs of hands — areas typically affected by chronic sun exposure. Women can frequently develop squamous cell carcinoma on their lower legs. This type of cancer is much more common in people who have a suppressed immune system due to other medical conditions or medications. Because squamous cell carcinoma spreads and grows faster than basal cell carcinoma, regular self-checks and continued monitoring by your dermatologist are vital for early detection and prompt treatment.
A squamous cell carcinoma can begin as a precancerous, scaly lesion (actinic keratosis) and then progress to a true skin cancer. They are often firm, round and tender to the touch. They grow more quickly than basal cell carcinoma and sometimes spread to other parts of the body. When treated promptly, squamous cell carcinoma are usually highly curable.
How to Prevent Squamous Cell Carcinoma
Ultraviolet light is the most preventable risk factor for all types of skin cancer, including squamous cell carcinoma. Protect your skin from UVA/UVB rays anytime you’re outdoors by:
- Apply sunscreen
Be sure to use a broad-spectrum sunscreen of SPF 30 or higher
- Re-apply sunscreen
A good rule of thumb is to re-apply suncreen every two hours or after swimming or sweating
- Be smart about being in the sun
Wear a wide-brimmed hat and sun-protective clothing, and plan to enjoy the outdoors during non-peak sunlight hours
- Avoid tanning beds
Avoid tanning beds, which can cause premature aging and skin cancer
Squamous Cell Carcinoma Diagnosis
When you visit our office because you’ve noticed a suspicious-looking spot on your skin, your dermatologist will first perform a physical exam and gather information about your health history. Then, depending upon this evaluation, your dermatologist may remove a portion of the lesion if he or she suspects the potential for skin cancer. This is called a skin biopsy. A biopsy is essential because it’s the only way to determine the presence of skin cancer with 100 percent certainty.
A pathologist will examine the skin your dermatologist has removed under a microscope, looking for skin cancer cells. The pathologist will then provide a biopsy report to your dermatologist to direct our next steps of treatment
It can take one to two weeks for your dermatologist to receive and review your biopsy report. These results will guide further followup or treatment. If a diagnosis of skin cancer is confirmed, we will help you determine the most appropriate course of care.
Squamous Cell Carcinoma Treatment
When diagnosed and treated early, most squamous cell carcinomas are highly treatable either with relatively minor surgery or occasionally with topical medication. Prompt treatment following diagnosis is important. In more advanced stages, squamous cell carcinoma can become more difficult to address, with the potential to spread to local lymph nodes, distant tissues and organs.
The best treatment for your squamous cell carcinoma depends on the size, location and aggressiveness of the tumor, in addition to your own preferences.
If your cancer is very small and/or superficial and presents a low risk of spreading, your dermatologist may recommend one of the following less-invasive treatments:
- Curettage and electrodessication (C and E) Removing the surface of the skin cancer with a scraping instrument (curet) and then searing the base of the cancer with an electric needle.
- Laser therapy. An intense beam of light vaporizes growths, usually with little damage to surrounding tissue and with a reduced risk of bleeding, swelling and scarring.
Your dermatologist may recommend more invasive treatments for larger squamous cell carcinoma that extend more deeply into the skin. Treatment options could include:
Simple excision. Your dermatologist would remove the cancerous tissue and a surrounding margin of healthy skin. In some cases, your doctor may recommend removing additional (non-cancerous) skin surrounding the tumor (wide excision).
Mohs surgery. During Mohs surgery, the surgeon will remove the visible cancerous tissue, then excise and examine microscopic samples of the tissue around it. They repeat this process until the samples — and you — are cancer-free.
Radiation therapy. Radiation therapy is sometimes used after surgery when there is an increased risk that the cancer will return. It might also be an option for people who can’t undergo surgery.
For squamous cell carcinomas that have spread beyond the skin, your dermatologist may coordinate with other providers to provide the very best care possible. Treatments may include chemotherapy, targeted drug therapy or immunotherapy.